
Your past does not have to define your future. This article outlines what trauma is, key differences between PTSD and Complex PTSD, and how to heal from trauma with counselling, including EMDR and Somatic Therapy.
“Healing involves discomfort. But so does refusing to heal. And over time, refusing to heal is always more painful.”
— Resmaa Menakem
Whether you have recently experienced something traumatic, are just beginning to understand your own history with traumatic experiences, or are seeking information to help a loved one — you’re in the right place.
My name is Taylor Evans. I’m a trauma therapist, mindfulness teacher, and writer passionate about supporting clients as they heal from their own trauma narratives. I believe trauma can present itself in a variety of ways and through different origin stories.
For many, experiences of trauma are buried — whether by self, family, or people we trust. My wish for you is to unburden yourself from the pain of aloneness, and let someone hold this with you for awhile. Telling someone you love, or working with a trauma-informed therapist are two great places to start.
What is Trauma?
Most individuals come to counselling with some trauma history. In media, trauma is often depicted as a single, life-threatening event — like surviving a disaster, sexual assault, or car accident. While of course these are examples of traumatic events, the scope of what we as a culture consider to be traumatic is broadening.
A trauma history can also include: childhood emotional neglect, undergoing surgery, enduring an emotionally, physically, or verbally abusive relationship, being Indigenous, Black, or a Person of Colour in North America, being houseless, child birth, divorce or uncoupling, on-going war or political unrest, exiting a high-control religion, loosing a loved one, and more.
A traumatic event is anything that exceeds our ability to cope. With the following caveat — our culture has trained us to “cope” with more than most bodies are capable of. In a culture of toxic positivity we are excellent as gaslighting ourselves; forcing ourselves to be strong and stay positive, all under the guise that “it’s not that bad, other people have it worse.” However, there is no limit on empathy, or moral prize for diminishing our struggles.
For this reason, the impact of trauma can be insidious. We might experience an event, or season of traumatic experience, and not recognize the impact of it until months, or even years later. Trauma also has a compounding effect, meaning it builds up over time if not addressed.
PTSD and C-PTSD
Our understanding of trauma is just beginning to take root in Western practice. The acknowledgement of trauma and trauma healing practices has been recognized since time immemorial by Indigenous communities and Eastern cultures.
Receiving a diagnosis can bring up complex emotions: they can be empowering, or disempowering, attached to stigma, and they can also be validating. As a clinical counsellor I’m unable to provide definite diagnoses to clients, however, a clinical idea of what a client is experiencing can help with treatment — it can provide a roadmap to therapy.
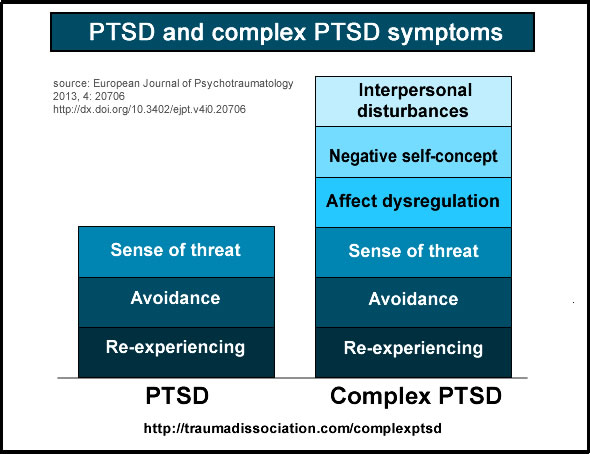
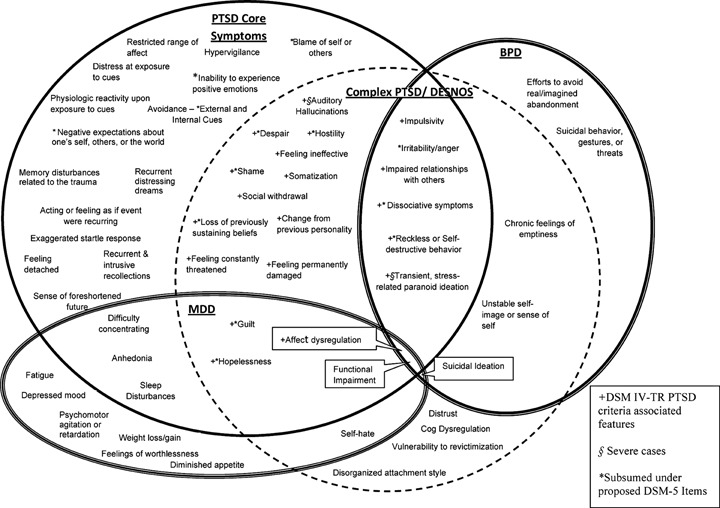
It can be helpful to know the signs of Post-traumatic Stress Disorder (PTSD). C-PTSD, or Complex Post-traumatic Stress Disorder, often includes the traditional markers of PTSD, as well as emotional dysregulation, negative self-concept and negative self-talk, and difficulties in relationships.
Trauma can also intersect with diagnoses of Borderline Personality Disorder (BPD). This is why it’s important for counsellors to take a trauma-focused approach when supporting clients with BPD.
Treating PTSD and CPTSD
When healing PTSD and CPTSD, it’s important to take a 3 phase approach. The 3 phases of trauma-focused therapy are: 1) Safety, Stabilization and Education, 2) Processing and Integration (also called Remembrance and Mourning), and 3) Connecting with Others and Self. The 3 phasic approach to healing trauma was popularized by both Pierre Janet and Judith Herman.
The following are approaches to healing from the aftermath of trauma. This is not an exhaustive list, rather, it’s a list informed by my approach to treating trauma.
My approach to treating trauma is both body-based and relational. This suggests two key underpinnings:
- Trauma is experienced in the body.
- Trauma often occurs in relationship to other people.
Other cognitive-based approaches include: Trauma-Focused CBT, Cognitive Processing Therapy, and Exposure Therapy.
EMDR
Eye Movement Desensitization Therapy (EMDR) is a well validated approach to treating trauma. EMDR uses Bilateral Stimulation (BLS) to stimulate the right brain and the free association of memory, emotion, sensation, and thought.
The right brain is often referred to as the emotional brain. Emotion plays a major role in the imprinting of traumatic events, and in our experience of life and self after. By tapping into emotion and our ability to connect with different layers of our experience (images, feelings, sensations, and thoughts) we’re able to process the past and reinforce positive experiences with a higher level of richness and depth.
Somatic Therapy
Somatic Therapy is an umbrella term for many body-based approaches to healing. Some of the most popular Somatic Therapy methods include: Somatic Experiencing, Sensorimotor Psychotherapy, and even EMDR. For the purpose of this article, I’ll focus on Somatic Experiencing (SE).
Somatic Experiencing teaches somatic skills based on increasing one’s body awareness and capacity to be with difficult emotions and sensations. By being with difficult emotions and sensations, the individual is able to fully process the past, and complete different stress responses held in the body.
At the same time, Somatic Experiencing helps people increase their capacity to be with the good parts of life. This is called Resourcing (one of SE’s somatic skills), and it’s a technique that helps clients learn to hold duality. While there can be pain, there can also be goodness, love, and pleasure!
Attachment-Focused
Trauma often occurs in relationship to other people. This causes a rupture, or attachment wound. In Attachment-focused therapy, we seek to repair the rupture through a variety of avenues. This might look like learning or re-learning how to co-regulate with others, or self-soothing if we experience an over reliance on others.
